ARTICLE Categories
All
|
|
Foods, ingredients, or molecule intolerances appear to be on the rise and whilst some such as gluten or histamine are well known, others, such as salicylates, are more misunderstood. This article will delve into this lesser-known phenomenon exploring:
What are salicylates and what is a salicylate intolerance? Salicylates are natural chemicals found in many plants who use them to defend themselves against pests, bacteria, and environmental stressors. Salicylates are anti-inflammatory and as such have also been synthetically reproduced in laboratories for uses in medications, including aspirin and non-steroidal anti-inflammatories (NSAIDs) such as ibuprofen. Salicylic acid has excellent anti-fungal and anti-bacterial properties, leading to its common use as an ingredient in processed foods, condiments, cosmetics, and beauty products. In terms of food, salicylates are found in many plant foods to a higher or lesser extent. Some of the foods that are common triggers are:
Salicylate intolerance is where a person’s system has difficulty metabolising and tolerating salicylates, leading to a range of symptoms. The phenomenon was initially observed in medically diagnosed patients with either aspirin-exacerbated respiratory disease (AERD) or NSAIDs-exacerbated respiratory disease (NERD) (1,2). In the cases of both AERD and NERD, high doses of chemical salicylates can trigger asthma, rhinosinusitis and urticaria. Clinical case studies have observed that for some, simply eating a diet high in salicylates can contribute to a variety of symptoms, although this can vary from person to person and may also depend on the quantity of salicylates eaten or exposed to over a short period of time. Which symptoms are linked to salicylate intolerance? Whilst respiratory and skin symptoms are the most recognised symptoms of salicylate intolerance, there are others including:
What does the science say causes this condition? As with so many conditions, the exact cause of salicylate intolerance is not well understood, however there are some areas which are being explored:
How is salicylate intolerance medically diagnosed? Diagnosis of salicylate intolerance is tricky, mainly because of the number of overlapping symptoms with other conditions. A medical or nutrition practitioner will undertake:
For many, a salicylate intolerance is linked to other conditions or genetics and is not, itself, the root cause. Sufferers tend to go heavily down the elimination root, which whilst does initially provide relief, is not a sustainable or healthy long-term solution. Working with a practitioner to discover the main trigger of the sensitivity is key. Suggestions for managing a suspected salicylate intolerance.
If on medication, please speak to your GP/consultant before making any changes to your diet. Sign up for my news to receive the published articles straight to your inbox. Read more by clicking below to see my previously published articles:
I’m Jessica Fonteneau, the Eczema and Digestive Health Nutrition Expert. I’ve worked with hundreds of clients to help them change their diets, better manage their flares, and find relief. My vocation is to help those with eczema and digestive issues, because I have suffered with these interlinked conditions since I was 6 months old, and I truly know what it is like to experience these debilitating conditions. Every client I have ever worked with has their own triggers and ideal nutrition. There is no such thing as ‘one-size-fits-all’. Whether you work with me one-to-one or use my guided tools, my objective is to help you uncover what works best for you, so that you take back control and experience relief. My guided programmes are only suitable for adults as children have very specific nutrition requirements. I do, however, work with many child clients as part of my clinic. I also offer two free communities for adults caring for children with eczema and digestive symptoms, feel free to come and join us and get some well-deserved support.
To easily keep up with my articles, masterclasses, ebooks and online programmes and receive exclusive access to early bird offers, sign-up to my newsletter. Interested in what I do and who I am? Go to my website: www.jessicafonteneaunutrition.com References:
0 Comments
The trees begin to lose their leaves, and you sigh a great sigh of relief thinking that the hay fever and seasonal allergies season is finally over. Then you realise that you are still getting symptoms – itchy eyes, runny nose, a dermatitis flare. It is very possible and even probable that you are suffering from Autumnal allergies.
TV adverts and magazine articles would have you think that hay fever and seasonal allergies only happen in the spring and summer, but that isn’t the case. Autumn brings its own set of allergens ready to trigger a runny nose, atopic dermatitis, and itchy eyes. If it isn’t plant pollen, what are the autumnal triggers that can cause so many issues? Weed pollen, mould spores and house mites are the most common triggers for Autumnal allergies, read on to find out more details and to get my 5 tips to lessen the autumnal allergy symptoms. Weed Pollen Not all pollen producing plants flower in spring. A whole category of weeds flower in the autumn and produce the highly allergenic weed pollen. These plants usually flower from late August until the first frost (usually around the end of November but growing later with climate change). This category of plants includes common weeds found in the UK such as nettles and sorrel but also varieties that are much newer to the UK and Europe such as the American Ragweed. Not only is ragweed a recent invader, but it also produces one of the highest amounts of pollen, causing uncomfortable hay fever and dermatitis symptoms in many sufferers. Mould Spores Mould is around us all the time, but at this time of year levels peak with the falling leaves gently composting on the ground releasing large amounts of allergenic spores. These are the main types of mould which have been highlighted as being triggers for allergy symptoms: Cladosporium Herbarum – this is a black mould that you can sometimes be found on bathroom walls or in a fridge, but it is also found on rotting vegetation. This is the considered the most allergenic of the moulds as it is easily airborne and so can spread quickly. Penicillium Notatum – found in decomposing leaves and soil. This mould is also the type you find on food that is going off eg. bread and fruit. Alternaraia Alternata – mainly found in rotting wood and therefore, forests, but can also be present on food and textiles. Dust Mites Many sufferers of asthma, eczema or hay fever also have a dust mite allergy and whilst dust mites exist all year, reactions tend to peak in autumn as the weather becomes damp but remains relatively warm and we retreat inside and close our doors and windows, but we haven’t yet put our heating on. 5 Tips to Lesson the Autumnal Allergy Symptoms
If you were interested in this article, you may be interested in these other blogs I’ve previously published: Sign up for my news to receive the published articles straight to your inbox. Read more by clicking below to see my previously published articles:
I’m Jessica Fonteneau, the Eczema and Digestive Health Nutrition Expert. I’ve worked with hundreds of clients to help them change their diets, better manage their flares, and find relief. My vocation is to help those with eczema and digestive issues, because I have suffered with these interlinked conditions since I was 6 months old, and I truly know what it is like to experience these debilitating conditions. Every client I have ever worked with has their own triggers and ideal nutrition. There is no such thing as ‘one-size-fits-all’. Whether you work with me one-to-one or use my guided tools, my objective is to help you uncover what works best for you, so that you take back control and experience relief. My guided programmes are only suitable for adults as children have very specific nutrition requirements. I do, however, work with many child clients as part of my clinic. I also offer two free communities for adults caring for children with eczema and digestive symptoms, feel free to come and join us and get some well-deserved support.
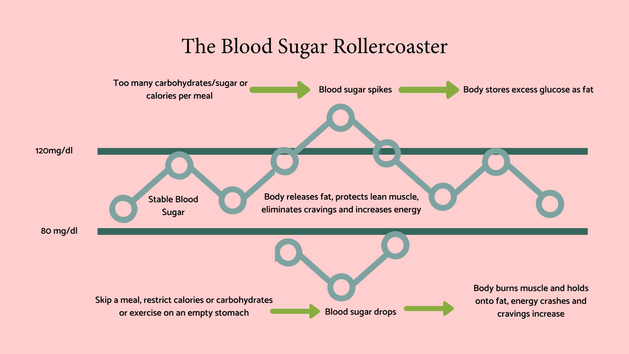
To easily keep up with my articles, masterclasses, ebooks and online programmes and receive exclusive access to early bird offers, sign-up to my newsletter. Interested in what I do and who I am? Go to my website: www.jessicafonteneaunutrition.com Blood sugars and continuous blood sugar monitors are all the rage and for good reason. Maintaining a stable blood sugar level isn’t just vital for metabolic health and weight, but also plays a key role in maintaining healthy skin and a normal functioning gut. This article will explore the connections between stable blood sugars and both skin and gut health and will provide practical tips to achieve and maintain this important balance:
The role of stable blood sugars Before we go into the detail of blood sugar and skin and gut health, here’s a quick overview of how important blood sugars are, so that we put it all in context. Simplistically, blood sugar is our main source of energy, and we get it primarily from eating carbohydrates which our digestive system then breaks down to glucose. This then enters our blood stream and provides energy to cells. Stable blood sugars are vital for lots of reasons, but here are the most cited ones:
Blood sugars and skin health
There are several ways that blood sugars can have an impact on skin health including:
Blood sugars and gut health Blood sugars and gut health aren’t usually associated by most people; however, high blood sugar levels can influence:
My top tips for keeping your blood sugars stable.
I run a 5 day ‘A Week to Reduce Your Sugar Cravings’ Challenge – it’s absolutely free and you can sign up here. Sign up for my news to receive the published articles straight to your inbox. Read more by clicking below to see my previously published articles:
I’m Jessica Fonteneau, the Eczema and Digestive Health Nutrition Expert. I’ve worked with hundreds of clients to help them change their diets, better manage their flares, and find relief. My vocation is to help those with eczema and digestive issues, because I have suffered with these interlinked conditions since I was 6 months old, and I truly know what it is like to experience these debilitating conditions. Every client I have ever worked with has their own triggers and ideal nutrition. There is no such thing as ‘one-size-fits-all’. Whether you work with me one-to-one or use my guided tools, my objective is to help you uncover what works best for you, so that you take back control and experience relief. My guided programmes are only suitable for adults as children have very specific nutrition requirements. I do, however, work with many child clients as part of my clinic. I also offer two free communities for adults caring for children with eczema and digestive symptoms, feel free to come and join us and get some well-deserved support.
To easily keep up with my articles, masterclasses, ebooks and online programmes and receive exclusive access to early bird offers, sign-up to my newsletter. Interested in what I do and who I am? Go to my website: www.jessicafonteneaunutrition.com References:
Histamine intolerance is a recently identified but increasingly considered condition that, whilst not life-threatening, can trigger a range of uncomfortable and often debilitating symptoms. The disparity and variety of symptoms that can be attributed to this condition are so widespread that it took time for the scientific community to observe the common denominator, and it is often misdiagnosed in general practice. This, the fifth and last article in my ‘histamine’ series, will delve into this condition that is grabbing the attention of the healthcare community, providing you with information that may help you unravel whether histamine intolerance may be a factor in your health. The article covers:
What is histamine intolerance? Histamine intolerance, also known as histaminosis or histamine sensitivity, is an increasingly recognised condition that affects a significant number of people worldwide. (1,2) is usually defined as the inability to adequately breakdown histamine. Histamine is a neurotransmitter, found throughout the body, but specifically in the skin, respiratory tract, and the digestive system. It is involved in numerous processes including stomach acid production, and vasodilation (the widening of the blood vessels), but is more commonly known for its pivotal involvement in the immune response. It is believed that individuals who suffer from histamine intolerance have a deficiency or dysfunction of the DAO (diamine oxidase) or HNMT (histamine-N-methyltransferase, enzymes, which are responsible for breaking down histamine in the body. This slowing of histamine degradation leads to a possible accumulation of histamine, leading to a variety of symptoms, depending on the individual. It is thought that histamine intolerance prevalence is higher in children than in adults (3), but further studies are needed. My clinical experience, working with many infants and young children with digestive and skin symptoms, is that when true IgE allergies have been ruled out, histamine intolerance is often a route to be explored. Lowering an overall histamine load, rather than assuming that multiple food intolerances are at play, can allow children to retain the all-important macro and micronutrient variety, rather than putting them at risk of strict and restrictive elimination diets which oftentimes worsens the situation and puts their health at risk. Histamine intolerance has, in the past, often been misdiagnosed as whole host of other diseases including food allergy and intolerances, urticaria, eosinophilic gastroenteritis amongst others. When clients come to see me with negative allergy/intolerance testing, but who swear blind that such and such a food triggers a reaction, histamine intolerance is something that immediately springs to mind. Which symptoms hint at a possible histamine intolerance? As I’ve already explored in previous articles (see links at the end of this feature), histamine intolerance can manifest in a variety of different symptoms, hence the diagnosis difficulty. Common symptoms include:
What are the possible contributory causes? There are several possible contributory causes to histamine intolerance, but the main theory involves the concept of an overall histamine ‘load’ or the cumulative effect of several factors, including:
Please note that not every individual will be affected by all the above, and this overview should only support the notion of how your overall histamine load could add up. The genetics of histamine intolerance For some experiencing histamine issues, the question of low or slow DAO or HNMT activity may stem from their genetics. DAO inactivates histamine in the gut and HNMT within the nervous system and lungs. Genetic variants on these enzymes or their pathways can lead to histamine intolerance. Nutrigenomics testing, which I offer through Lifecode Gx, can provide information on our own genes which then informs us on the nutrition and lifestyle changes we can make to align with any variants to optimise health and wellbeing. Lifecode Gx offers a specific Histamine Intolerance test. You can find out more, by clicking the link. Nutrigenomic testing is the only form of testing that is available from the youngest age. Whilst how you eat and live your life will have an effect on whether a gene variation may have an impact, your genes themselves never change. My top tips for lowering your histamine load.
If on medication, please speak to your GP/consultant before making any changes to your diet. If you are interested in histamine and its impact on symptoms, this article is the second in a series I am currently publishing covering. The series in total will include:
Sign up for my news to receive the published articles straight to your inbox. Read more by clicking below to see my previously published articles:
I’m Jessica Fonteneau, the Eczema and Digestive Health Nutrition Expert. I’ve worked with hundreds of clients to help them change their diets, better manage their flares, and find relief. My vocation is to help those with eczema and digestive issues, because I have suffered with these interlinked conditions since I was 6 months old, and I truly know what it is like to experience these debilitating conditions. Every client I have ever worked with has their own triggers and ideal nutrition. There is no such thing as ‘one-size-fits-all’. Whether you work with me one-to-one or use my guided tools, my objective is to help you uncover what works best for you, so that you take back control and experience relief. My guided programmes are only suitable for adults as children have very specific nutrition requirements. I do, however, work with many child clients as part of my clinic. I also offer two free communities for adults caring for children with eczema and digestive symptoms, feel free to come and join us and get some well-deserved support.
To easily keep up with my articles, masterclasses, ebooks and online programmes and receive exclusive access to early bird offers, sign-up to my newsletter. Interested in what I do and who I am? Go to my website: www.jessicafonteneaunutrition.com References:
Upcoming programmes and eventsClick on the thumbnails to find out more
|
AuthorI’m Jessica Fonteneau, I’m the eczema specialist and I help people Escape from the Eczema trap. Archives
April 2024
Catégories
All
|




 RSS Feed
RSS Feed