ARTICLE Categories
All
|
|
You’ve probably heard that Vitamin D is important, but did you know that it can be critical if you suffer from eczema/dermatitis?
This is why one of the first questions I ask clients is whether they know their Vitamin D3 status. Do you know yours? If you want to know more about how vitamin D or the lack thereof might be influencing your skin health, read on. Today’s article covers:
What is vitamin D3 and why is it important? Vitamin D3 starts off as cholecalciferol which we, in the main, absorb through our skin through UVB or sunlight exposure. The cholecalciferol then goes through numerous processes in the liver and kidneys to become what is known as a biologically active form, or a form that our body can easily use, calcitriol. Vitamin D3 is, in fact, more of a hormone than a vitamin and it acts as a signaller to tell hundreds of genes what to do. We have Vitamin D Receptors (VDR) throughout our body that are just waiting for the calcitriol to come and bind with them. This binding of the calcitriol and the VDR triggers a cascade of vital bodily processes via genes from bone health and calcium metabolism to inflammation and heart health amongst many others. Vitamin D is most known for its effects on bone health as it helps calcium and phosphorus be absorbed from the gut, essential for the building and formation of strong bones. Low Vitamin D levels are linked to weak bones (Rickets) in children and osteomalacia (bone softening) in adults. (1) Vitamin D is known to have anti-inflammatory properties, which is very useful if you are prone to inflamed skin as most eczema/dermatitis sufferers are. (2) Vitamin D is thought to be important for heart health including hypertension and also brain health, due to the vast number of VDRs that can be found in brain tissue. (3) How gene variations can have an impact on your Vitamin D levels Gene variations you may have can, in some cases, impact on vitamin D availability or how responsive your receptors are to receiving the calcitriol. If a client comes to me and says that their Vitamin D3 levels are always low, then I would suspect a genetic variant at play either on the GC gene which controls supply of Vitamin D Binding Protein (VDPR) important for transporting Vitamin D around the body or variances on the VDR gene itself, meaning that receptors are less keen to receive and bind to the circulating Vitamin D. Another gene variation linked to Atopic Eczema is filaggrin. Vitamin D influences the production and function of skin proteins including filaggrin, so maintaining your Vitamin D levels if you suffer from atopic dermatitis is especially important. Nutrigenomics testing can be helpful to see gene variances in relation to things like Vitamin D, inflammation or susceptibility to lactose or gluten intolerance amongst many others. I use Lifecode Gx as they provide a variety of reports that can help me unravel a great deal about an individual’s genes and how they are impacting their skin health. Vitamin D and its specific role in Atopic Dermatitis/Eczema Vitamin D is also vital for the growth and repair of skin cells. It supports your skin barrier, which means that it is more resistant to attacks, and it has anti-inflammatory properties that are, as I’ve already mentioned, crucial for skin conditions like dermatitis and psoriasis. The interesting thing is that the science is clear. If you have eczema, it is very likely that your Vitamin D test results will show that you are Vitamin D deficient. Atopic Eczema sufferers specifically are more likely to be more Vitamin D deficient than the normal population. Have you tested your levels recently? How can Vitamin D help if you have dermatitis/eczema? Research has shown that maintaining vitamin D levels can lead to a significant reduction in eczema symptoms, especially inflammation and infection. This is especially clear in the winter months when exposure to sunlight is so much lower. Many of my clients report that their skin naturally improves in the summer months. (4) As mentioned above, vitamin D helps keep your skin water and infection ‘tight’ thanks to its action on filaggrin, amongst other skin proteins. If your skin is ‘leaky’ you are more at risk of infection or even allowing a contact allergen to trigger a flare. A healthy skin barrier helps retain moisture as well, and we all know how much moisture a dermatitis sufferer needs to retain ! (5) How you can ensure that you are getting enough, whilst being careful to not have too much. As you may have noticed throughout the article, an optimal (serum) level of Vitamin D3 is vital for health but is also critical for skin health and eczema. Good sources of Vitamin D3 include:
It is important to note that more is not necessarily better. Too much Vitamin D, specifically from supplementation, can be dangerous for your health. If in any doubt check with a health or nutrition practitioner and test to see where your starting levels are. Sign up for my news to get useful, usable information, resources and offers straight to your inbox. References.
0 Comments
Navigating Periorificial Dermatitis. Insights and Management Strategies for Adults and Children3/14/2024 Periorificial dermatitis is a broad term encompassing various skin conditions that affect the face, including perioral dermatitis. (1,2).
Today’s article aims to shed light on periorificial dermatitis, its types, symptoms, and triggers, with dedicated insights for both adults and children. Treatment and care as well as the impact of nutrition on its management will also be explored. What is periorificial dermatitis? Periorificial dermatitis is a common, yet often misunderstood skin condition, presenting as rash around the orifices or openings of the face and on the forehead. The different types are:
What are the common symptoms? This condition can be both physically uncomfortable and emotionally distressing. Common symptoms in adults include:
In children periorificial dermatitis is more challenging to diagnose due to overlapping symptoms with other paediatric skin conditions including atopic, contact eczema or even impetigo. Common triggers Common triggers include, but are not exclusive to:
Treatment and Care Medical diagnosis typically involves a clinical examination with a GP or dermatologist. The primary approach to care involves identifying and eliminating triggering factors, such as specific skincare ingredients, environmental irritants or even foods. For adults, medical treatment often includes topical immunomodulators, antibiotics or mild corticosteroids, however studies have shown that with this form of dermatitis the best course of action is often to leave well alone and not apply any creams at all. Recommendations focus on restoring the skin barrier along with a gentle, hypoallergenic skin care regime, alongside stress management and dietary changes. Paediatric management focuses on gentle cleansing and application of hypoallergenic moisturisers to maintain skin hydration. Avoiding known irritants, allergens and intolerances is key, especially if the child has an atopic terrain. I recently worked with an infant whose perioral dermatitis resolved up to 90% with the elimination of one trigger food. The role of nutrition in managing periorificial dermatitis There is no specific diet that focuses on modulating periorificial dermatitis, but nutrition can play a pivotal role in skin health, providing the correct nutrients to modulate inflammation, support natural immune function and strengthen both the gut and skin microbiomes.
Periorificial dermatitis can be challenging but can also be managed with the right approach encompassing medical solutions with lifestyle and nutrition modifications. Understanding the different types of periorificial dermatitis and recognising the importance of nutrition as the foundation to skin health are key steps towards achieving clearer, healthier skin. If you haven’t yet been diagnosed it’s essential to consult with your GP or dermatologist for an accurate diagnosis. Remember, nutrition is just one piece of the puzzle, even if it is a vital one. Skin/Gut Masterclass – Tuesday 19th March 2024 at 12pm UK time. If you are interested in hearing more about the skin/gut connection I am holding a Masterclass this coming Tuesday, 19th March at 12pm UK time. If you register and are unable to attend, you will receive a recording of the event on Wednesday 20th March. You can register here. References
Mast Cell Activation Syndrome (MCAS) is a complex condition that has been gaining attention in the medical community for its role in a variety of symptoms and diseases, including skin conditions such as eczema and dermatitis. (1–3) This article aims to shed light on what MCAS is, how it’s diagnosed, its connection to skin conditions and potential management strategies. What is MCAS? MCAS is a condition where mast cells, a type of white blood cell that play a crucial role in the body’s immune response, behave abnormally, triggering immune related symptoms. Mast cells play a pivotal role in the management of inflammatory responses, acting as the defensive guardians against pathogens. These cells are found in tissues throughout the body, especially where the body is exposed to contact with foreign bodies, such as the skin, lungs, and digestive tract. When mast cells detect a foreign substance or an injury they release a variety of different chemical signals including histamine, cytokines, and growth factors, which are all part of the body’s defence systems. This is normal and what keeps us healthy. Normally, mast cells help protect the body from disease and aid in wound healing but in MCAS these cells are overly sensitive and release too many of these chemicals leading to a range of symptoms that can affect every part of the body, including the skin, gastrointestinal, cardiovascular, respiratory and neurological systems. Long COVID is also thought to involve aspects of MCAS. Symptoms and Diagnosis The range of symptoms involved in MCAS are vast and can vary significantly from one individual to another. Reported symptoms include: flushing, itching, urticaria (hives), stomach pain, nausea, vomiting, diarrhoea, low blood pressure, headaches and breathing issues. The severity of symptoms can range from mild to life-threatening. As you can tell these are symptoms that can overlap with many other conditions making diagnosis tricky. Officially there are three sets of criteria needed for MCAS diagnosis:
The MCAS, Dermatitis Connection The skin is one of the organs most commonly affected by MCAS and dermatitis (atopic, contact and urticaria) is the most common skin illness linked to this condition. Dermatitis, characterised by inflammation of the skin, can be exacerbated by the overactive release of histamine and other chemicals from mast cells, leading to redness, itching, and swelling, all symptoms so characteristic of this chronic skin condition. The different types of eczema/dermatitis have multifactorial root causes including genetic, environmental and immune system factors. The link between MCAS and dermatitis is found within the immune system, particularly in how mast cells can over secrete the chemicals that can exacerbate an existing flare or trigger a new one. A combination of MCAS with chronic, relapsing dermatitis can cause misery for sufferers. Histamine, one of the most well-known mediators released by mast cells, is involved in immediate allergic reactions and plays a significant role in vasodilation or increased blood flow, and recruitment of other immune cells to the site of injury or infection. If you are interested in learning more about histamine, I have written a series of 5 articles relating to histamine, which can all be found via my website. Understanding the role of mast cells in immune responses and their contribution to conditions like MCAS and dermatitis underscores how intertwined both the immune system and skin health is. What is important to bear in mind is the need for support that may modulate mast cell activity but also alleviate the dermatitis symptoms. Management strategies for MCAS-Related Dermatitis Managing diagnosed MCAS and dermatitis needs a rounded approach that takes into account both the overactive mast cells and the dermatitis symptoms. Here are some tips that may help:
In summary, MCAS is a multifaceted condition that can significantly impact the physical and mental wellbeing of affected individuals. Having a medical diagnosis that then provides an appropriate treatment plan that alleviates symptoms is important, however, understanding the root cause of the hyper-activation be it food, environmental, lifestyle factors or stress is vital for long-term health. References.
Sign up for my news to receive the published articles straight to your inbox. Read more by clicking below to see my previously published articles:
I’m Jessica Fonteneau, the Eczema and Digestive Health Nutrition Expert. I’ve worked with hundreds of clients to help them change their diets, better manage their flares, and find relief. My vocation is to help those with eczema and digestive issues, because I have suffered with these interlinked conditions since I was 6 months old, and I truly know what it is like to experience these debilitating conditions. Every client I have ever worked with has their own triggers and ideal nutrition. There is no such thing as ‘one-size-fits-all’. Whether you work with me one-to-one or use my guided tools, my objective is to help you uncover what works best for you, so that you take back control and experience relief. My guided programmes are only suitable for adults as children have very specific nutrition requirements. I do, however, work with many child clients as part of my clinic. I also offer two free communities for adults caring for children with eczema and digestive symptoms, feel free to come and join us and get some well-deserved support.
To easily keep up with my articles, masterclasses, ebooks and online programmes and receive exclusive access to early bird offers, sign-up to my newsletter. Interested in what I do and who I am? Go to my website: www.jessicafonteneaunutrition.com In my 10 years in clinic, specialising in skin health, I’ve seen first-hand the profound impact diet and lifestyle choices have on skin health. One area that is increasingly grabbing attention is the skin microbiome and its role in conditions like dermatitis/eczema.
In this article I’ll explore what the skin microbiome is, its connection to dermatitis and how paying it some attention can be a crucial step in managing this challenging condition. The skin microbiome: Our body’s first line of defence. You’ve probably heard of the gut microbiome, the population of microorganisms, including bacteria, fungi and viruses that live in our gut, but you may not have heard of the skin microbiome. The skin microbiome has a similar community of microorganisms that live on our skin and this complex ecosystem is vital in the protection of our skin from harmful pathogens, inflammation regulation and overall skin health. The skin microbiome is not only part of the skin barrier that stops unwelcome organisms from entering the blood stream, but it also acts as a crucial go-between from the outermost skin layer and the immune system. It is crucial that a balance of microorganisms be maintained to support the health of any organ that has a microbiome, including skin and gut. When an imbalance occurs in the skin microbiome, skin conditions such as eczema can emerge or worsen. Eczema and Microbiome Balance Eczema, also known as dermatitis, is characterised by dry, itchy, and inflamed skin. Research has shown that individuals with eczema often have an altered or unbalanced skin microbiome. (1,2). Eczema patients frequently have an increase in the Staphylococcus aureus bacteria which plays a role both in inflammation and possible infection. This imbalance can disrupt the skin’s barrier function, making it more susceptible to irritants and allergens, further worsening eczema symptoms. Nurturing the Skin Microbiome The good news is that we can nurture our skin microbiome, just as we can support our gut bacteria population. Here are some tips to get you started:
1. Barbarot S, Aubert H. Physiopathologie de la dermatite atopique. Ann Dermatol Venereol. 2017;144:S14–20. 2. Nakatsuji T, Gallo RL. The role of the skin microbiome in atopic dermatitis. Ann Allergy, Asthma Immunol [Internet]. 2019;122(3):263–9. Available from: https://doi.org/10.1016/j.anai.2018.12.003 Sign up for my news to receive the published articles straight to your inbox. Read more by clicking below to see my previously published articles:
I’m Jessica Fonteneau, the Eczema and Digestive Health Nutrition Expert. I’ve worked with hundreds of clients to help them change their diets, better manage their flares, and find relief. My vocation is to help those with eczema and digestive issues, because I have suffered with these interlinked conditions since I was 6 months old, and I truly know what it is like to experience these debilitating conditions. Every client I have ever worked with has their own triggers and ideal nutrition. There is no such thing as ‘one-size-fits-all’. Whether you work with me one-to-one or use my guided tools, my objective is to help you uncover what works best for you, so that you take back control and experience relief. My guided programmes are only suitable for adults as children have very specific nutrition requirements. I do, however, work with many child clients as part of my clinic. I also offer two free communities for adults caring for children with eczema and digestive symptoms, feel free to come and join us and get some well-deserved support.
To easily keep up with my articles, masterclasses, ebooks and online programmes and receive exclusive access to early bird offers, sign-up to my newsletter. Interested in what I do and who I am? Go to my website: www.jessicafonteneaunutrition.com As I look out the window and watch the endless, pouring rain, I think of a dermatitis trigger that loves this type of weather, mould.
There have been quite a few truly tragic stories in the media over the past year, highlighting the devastating impact mould can have on health, particularly in relation to respiratory conditions, but did you even consider whether mould might be triggering your dermatitis flare? In this blog post, I’ll delve into the intricate relationship between mould exposure and dermatitis and explore ways to reduce the risks. A short mould overview. Mould refers to a type of fungus that thrives in damp and humid environments, basically the UK. Common indoor moulds include Aspergillus, Fusarium Stachybotrys chartarum and Clasporium Herbarum. Stachybotrys chartaruium and Clasporium Herbarum are visible as black mould, but some other moulds are practically invisible to the naked eye. Mould tends to develop in areas that are out of sight. Just this week, I had a message from a client who said “you know you were questioning me around mould, and I said that there absolutely wasn’t any in my home? Well, we’ve just changed the floor in our kitchen and guess what we found under the lino”. Moulds, including the infamous black mould, thrive in damp environments such as kitchens, basements, and bathrooms. They can grow on various surfaces, including paper, wood, and fabrics. When mould touches the skin, or when individuals with a mould sensitivity inhale the spores, it can trigger different types of skin rashes characterized by redness, itching, swelling, and sometimes small bumps or blisters. Dermatitis, what does it encompass? Dermatitis is a broad term encompassing a whole host of skin conditions from Atopic Eczema to contact dermatitis and even Cutaneous Aspergillosis a skin condition directly linked to the Aspergillus mould. The Mould/Dermatitis Connection Research has shown a compelling connection between mould exposure and development or worsening of dermatitis symptoms. People who live or work in damp environments with high mould concentrations have been observed to be more susceptible to skin issues. It is believed that contact, either directly or via minute mould spores landing on the skin or being breathed in, can trigger inflammation that leads to the symptoms so common in dermatitis or eczema: red patches, itching and often pain. The most common types of dermatitis linked to mould are:
Mycotoxins Mycotoxins are toxic compounds produced by some mould species and which add another complex layer to the mould/dermatitis connection. These substances can enter the body through inhalation, ingestion, or skin contact. When mycotoxins come into direct contact with the skin, they can disrupt the skin barrier function, leading to increased permeability or leaky skin and higher risk of skin irritations. Mycotoxins have been found to trigger rosacea, eczema and even acne. Immune Response As previously touched on, both mould and mycotoxin exposure can trigger an immune response, leading to both inflammation and skin reactions. Whilst dermatitis isn’t considered an autoimmune condition, the constant igniting of the immune response is tiring for the body and can lead, in turn, to increased susceptibility to infections and inflammation. An exhausting vicious cycle. Diagnosis If you suspect that mould is triggering your skin, then you should go and see your GP for a diagnosis. Blood tests, finger-prick or patch testing can determine whether mould is an issue for you. Common medical treatments include over-the-counter antihistamines and cortisone creams. Nutrition practitioners also have access to some functional tests which may be useful. Tips for Prevention If you have recurrent dermatitis and are at a loss as to why it is constantly triggered, then it may be worth exploring whether mould might be a cause:
Sign up for my news to receive the published articles straight to your inbox. Read more by clicking below to see my previously published articles:
I’m Jessica Fonteneau, the Eczema and Digestive Health Nutrition Expert. I’ve worked with hundreds of clients to help them change their diets, better manage their flares, and find relief. My vocation is to help those with eczema and digestive issues, because I have suffered with these interlinked conditions since I was 6 months old, and I truly know what it is like to experience these debilitating conditions. Every client I have ever worked with has their own triggers and ideal nutrition. There is no such thing as ‘one-size-fits-all’. Whether you work with me one-to-one or use my guided tools, my objective is to help you uncover what works best for you, so that you take back control and experience relief. My guided programmes are only suitable for adults as children have very specific nutrition requirements. I do, however, work with many child clients as part of my clinic. I also offer two free communities for adults caring for children with eczema and digestive symptoms, feel free to come and join us and get some well-deserved support.
To easily keep up with my articles, masterclasses, ebooks and online programmes and receive exclusive access to early bird offers, sign-up to my newsletter. Interested in what I do and who I am? Go to my website: www.jessicafonteneaunutrition.com www.facebook.com/groups/417030973601268This weeks’ article comes thanks to one of my members in my Free Facebook group for carers of children with gut and/or skin issues. She asked for exactly what it says in the title. Ideas for gently supporting gut health whilst appealing to a fussy eater.
At first glance it may appear that this article is only aimed at children, but it isn’t. You would be surprised how many adults have quite distinctive likes and dislikes when it comes to food. So, this is a great topic to tackle because it effects so many of us, whether we are a parent of a fussy eater, or whether we aren’t that keen on a few foods ourselves. Last thing before I delve properly into the topic. My belief is that fussy eaters are born and not made and so I want to take any of notion of guilt straight out of the equation. This is the little anecdote that brought me to that conclusion: My first-born loves all food, a lot. As an infant/young child he was never happier than when he was eating, and we were amazed by how adventurous he was, so young. I of course, as a first-time parent, foolishly thought that this had something to do with my parenting skills. As I was soon to find out, my son was born loving food, it had absolutely diddly squat to do with me. My daughter then arrived, and if I was a suspicious sort, I would think that she came specifically to teach me a lesson. Food didn’t interest her. She didn’t like lumps right from the start – baby porridge was a no-no, she just spat it out. She would only eat vegetables that came from tins, and she could outlast my patience at the table, by a considerable mile. She was born suspicious of most foods and there was nothing I could do to change it. Well, I did manage, but it took years. She is part of the reason I retrained as a Registered Nutritional Therapy Practitioner, I needed to know more, so I could feed her better. You’ll be pleased to hear that she now eats an amazing variety of foods and cooks for most of her friends. She still doesn’t like yogurts with ‘bits’, however. Anyway, enough digression. Today’s article is all about which nutrients are helpful to support gut health generally and some tips on how to subtlety incorporate them in the diet so that it slips past the most vigilant of fussy eaters. A quick overview of our digestive system and what it needs for health. Before we get into the nutrients and tips, just a quick overview of the gut. The gut runs all the way from our mouth to our bottom. Digestion starts in the mouth, specifically for carbohydrates (bread, pasta, flour-based products, potatoes etc), once swallowed the food passes via the oesophagus and is drip fed into the stomach. It then passes through into the small intestine, where most digestion of nutrients takes place, before moving into the large intestine where water is removed, and our gut bacteria continues to break down matter and synthesises certain vitamins. We then finally pass what’s left as a stool, and the process is complete. The whole process is managed thanks to peristalsis, a wave like action that helps propel the food to each area of the digestive stages. Many clients talk about gut problems, but that term is a little vague as issues can occur at any of the stages. We may eat too quickly and not chew enough so that the food is too large, and we experience a sensation that the food is hard to digest. We can have issues with our oesophagus so that some of the stomach acid comes up further than it should, and we experience reflux. We can have too much or even too little stomach acid so our foods, most commonly proteins, aren’t adequately broken down. We can have an issue with digestive enzymes or bile acids. Bacteria can come up to the small intestine, where they shouldn’t be and trigger small intestinal bowel overgrowth (SIBO). We can have an unbalanced gut bacteria population and constipation in the large intestine. So which nutrients are good for our digestive system? Here is a list of the nutrients, the tips on how to incorporate them will follow!
How to slip these ingredients into your fussy eater’s diet.
Sign up for my news to receive the published articles straight to your inbox. Read more by clicking below to see my previously published articles:
I’m Jessica Fonteneau, the Eczema and Digestive Health Nutrition Expert. I’ve worked with hundreds of clients to help them change their diets, better manage their flares, and find relief. My vocation is to help those with eczema and digestive issues, because I have suffered with these interlinked conditions since I was 6 months old, and I truly know what it is like to experience these debilitating conditions. Every client I have ever worked with has their own triggers and ideal nutrition. There is no such thing as ‘one-size-fits-all’. Whether you work with me one-to-one or use my guided tools, my objective is to help you uncover what works best for you, so that you take back control and experience relief. My guided programmes are only suitable for adults as children have very specific nutrition requirements. I do, however, work with many child clients as part of my clinic. I also offer two free communities for adults caring for children with eczema and digestive symptoms, feel free to come and join us and get some well-deserved support.
To easily keep up with my articles, masterclasses, ebooks and online programmes and receive exclusive access to early bird offers, sign-up to my newsletter. Interested in what I do and who I am? Go to my website: www.jessicafonteneaunutrition.com Irritable bowel syndrome (IBS) is a common functional gastrointestinal condition that affects millions of people in Western societies. Incidence of IBS is on the increase with more and younger people being diagnosed and experiencing symptoms including stomach pain, bloating and irregular bowel movements. Exact causes are unknown, and IBS remains the common diagnosis once all other digestive conditions have been ruled out. Ultra-processed foods and drinks (UPFD) are increasing in both consumption and visibility, but so too is the amount of evidence growing that highlights this food group’s problematic relationship with health. This article will explore the association between consumption of UPFDs and IBS and will give 5 tips on how to transition away from UPFDs if you suffer from IBS. A quick IBS overview IBS is a complex and often long-term (chronic) digestive disorder that effects the large intestine or colon. IBS is considered a functional gut disorder as there is no damage to the gut. Symptoms can vary from person to person, but include a combination of the following:
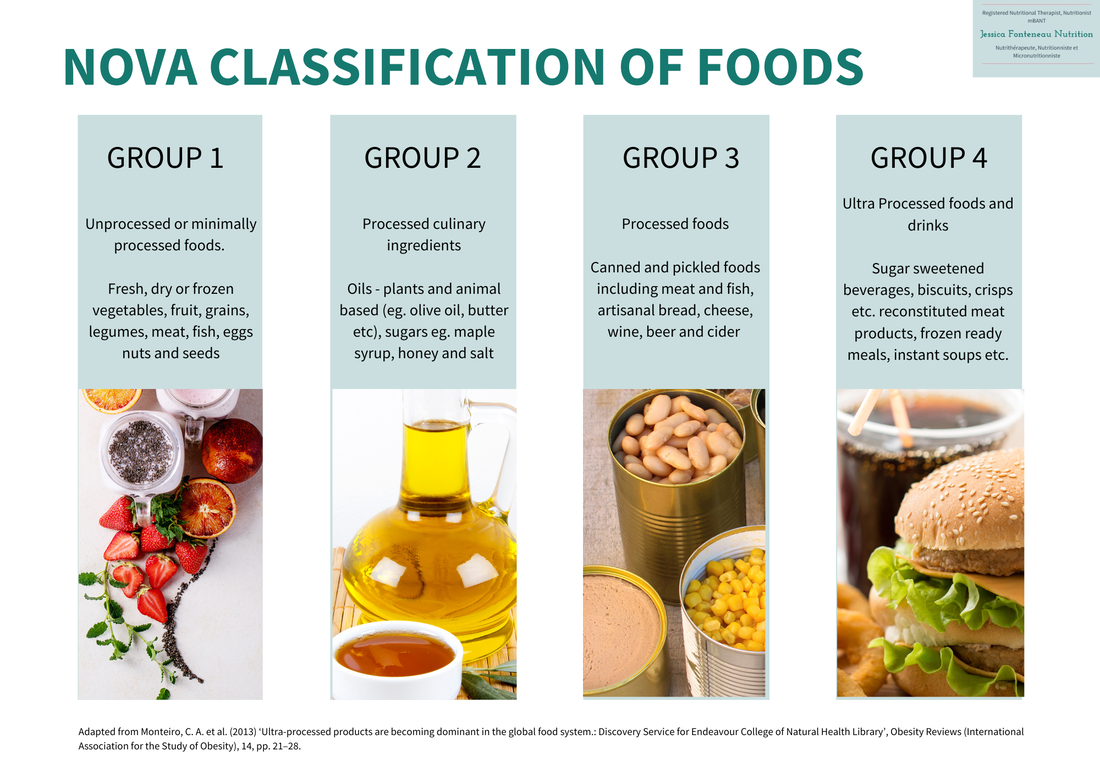
If you experience any of these symptoms, you should consult with a medical practitioner. IBS is thought to be caused by several triggers including gut motility (the movement of your stool through your gut), gut microbiome and gut hormones. Diet and stress have been identified as triggers for onset or worsening of IBS symptoms. Ultra-Processed Foods and Drinks. The jury is still out on the classification of what makes a UPFD, however since 2013 the NOVA classification developed by Monteiro et al., (6) has been the system most quoted. The NOVA classification divides products into four categories, from unprocessed or minimally processed foods to ultra-processed foods and drinks:
In a nutshell, UPFDs are highly processed products that usually contain a long list of additives, preservatives, and artificial ingredients. They can be found packaged in bright, colourful packaging and they are promoted as being convenient as well as being delicious and economical, as they usually have long shelf lives. How UPFDs affect gut health including IBS When a person is diagnosed with IBS, they are often recommended a low FODMAP diet which is fundamentally a very low fibre diet. Many of my clients come to me saying that ultra-processed foods are those that they tolerate the best on this way of eating. What they don’t realise is whilst these foods and drinks appear to be more easily digested, they are, in fact, reinforcing and exacerbating the problem. Studies have shown that the gut microbiome is different in those who regularly eat UPFDs and those that don’t. Those whose diet includes many UPFDs tend to have a larger population of gut bacteria that is considered more pro-inflammatory (triggers more inflammation). There are numerous ways in which UPFDs affect gut health and can contribute to IBS including:
5 Top Tips for Transitioning Away from Ultra-processed foods if you have IBS. Caution: someone with IBS who has been following a low FODMAP or low-fibre diet shouldn’t suddenly change their diet. I would strongly recommend that anyone wishing to modify their diet consult with a medical or nutrition practitioner.
Sign up for my news to receive the published articles straight to your inbox. Read more by clicking below to see my previously published articles:
I’m Jessica Fonteneau, the Eczema and Digestive Health Nutrition Expert. I’ve worked with hundreds of clients to help them change their diets, better manage their flares, and find relief. My vocation is to help those with eczema and digestive issues, because I have suffered with these interlinked conditions since I was 6 months old, and I truly know what it is like to experience these debilitating conditions. Every client I have ever worked with has their own triggers and ideal nutrition. There is no such thing as ‘one-size-fits-all’. Whether you work with me one-to-one or use my guided tools, my objective is to help you uncover what works best for you, so that you take back control and experience relief. My guided programmes are only suitable for adults as children have very specific nutrition requirements. I do, however, work with many child clients as part of my clinic. I also offer two free communities for adults caring for children with eczema and digestive symptoms, feel free to come and join us and get some well-deserved support.
To easily keep up with my articles, masterclasses, ebooks and online programmes and receive exclusive access to early bird offers, sign-up to my newsletter. References
There comes a time in most parent’s life when you are faced with your child complaining of stomach-ache and asking to stay home from school. I know, it happened to me frequently with my youngest daughter.
It can be so hard to judge, especially with younger children, whether the issue is serious or simply an appeal for a day off. My daughter has admitted that some of those earlier episodes were a case of her just wanting to stay home rather than face a test, but others were genuine. When her stomach aches started to interfere with her high-level sport practice, which she loved, I knew for sure that things weren’t right, and I consulted our GP who referred her to a gastroenterologist. In her case, all was well, but if you have any doubt about your child’s symptoms, consult your own medical practitioner. Whilst children’s stomach aches can be triggered by many things, for some it comes from Paediatric Irritable Bowel Syndrome (IBS) and this article will give an overview on:
Understanding paediatric IBS IBS, whether paediatric or adult, is a functional gastrointestinal disorder. That means that there is no physical damage to the gut, but rather a disorder in how the digestive system is working, which can lead to a range of distressing symptoms. Paediatric IBS often develops during adolescence, but some children develop the condition at a younger age. It is thought that up to 15% of the paediatric population suffers from this condition. The name Irritable Bowel Syndrome (IBS) can easily be confused with Irritable Bowel Disease (IBD) which encompasses Crohn’s and Ulcerative Colitis, but it is a completely different condition. Symptoms of paediatric IBS
Diagnosing paediatric IBS Any children with persistent symptoms should see their medical practitioner. It is worth being aware that diagnosing paediatric IBS can be challenging, because it overlaps with other gastrointestinal disorders, and it is usually diagnosed following a process of elimination via a combination of medical history, physical examination, and tests. If your family has any history of gastrointestinal disorders, then it is essential to share that information with your medical practitioner. Tips for how to support your child diagnosed with IBS.
IBS in children is a real, but often misunderstood condition that can have a significant impact on a child’s daily life. Recognising the symptoms, seeking healthcare advice for proper diagnosis and nutrition support, and introducing some anxiety relief techniques are crucial to help improve quality of life. Sign up for my news to receive the published articles straight to your inbox. Read more by clicking below to see my previously published articles:
I’m Jessica Fonteneau, the Eczema and Digestive Health Nutrition Expert. I’ve worked with hundreds of clients to help them change their diets, better manage their flares, and find relief. My vocation is to help those with eczema and digestive issues, because I have suffered with these interlinked conditions since I was 6 months old, and I truly know what it is like to experience these debilitating conditions. Every client I have ever worked with has their own triggers and ideal nutrition. There is no such thing as ‘one-size-fits-all’. Whether you work with me one-to-one or use my guided tools, my objective is to help you uncover what works best for you, so that you take back control and experience relief. My guided programmes are only suitable for adults as children have very specific nutrition requirements. I do, however, work with many child clients as part of my clinic. I also offer two free communities for adults caring for children with eczema and digestive symptoms, feel free to come and join us and get some well-deserved support.
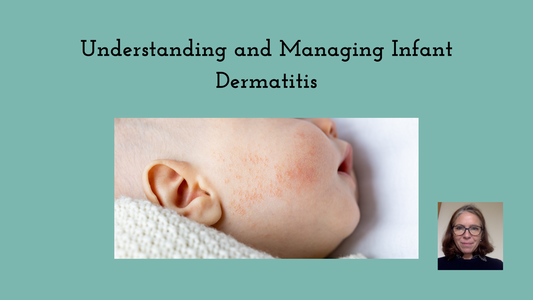
To easily keep up with my articles, masterclasses, ebooks and online programmes and receive exclusive access to early bird offers, sign-up to my newsletter. Understanding and Managing Infant Dermatitis Infant dermatitis is a common skin condition that affects babies in infancy. Whilst it can be distressing for both parents and babies, it’s vital to remember that most cases can be effectively managed with proper care and management. This article is aimed at parents whose infants have recently been diagnosed with dermatitis and will explore:
The different types of infant dermatitis
Causes There are different possible causes, depending on the type:
Role of Nutrition Nutrition is the foundation of all our cells, including skin cells and it can have an impact on the development and management of infant dermatitis. In the past allergens were strictly avoided in infants, but research has uncovered that this may make food allergies more prevalent. The guidelines, now are:
Nutrients that support healthy skin Some nutrients are essential for skin health generally, so if your infant is weaned and hasn’t demonstrated any allergies or intolerances, then consider including the following nutrients into their regular nutrition can be supportive:
My tips for managing infant dermatitis.
Sign up for my news to receive the published articles straight to your inbox. Read more by clicking below to see my previously published articles:
I’m Jessica Fonteneau, the Eczema and Digestive Health Nutrition Expert. I’ve worked with hundreds of clients to help them change their diets, better manage their flares, and find relief. My vocation is to help those with eczema and digestive issues, because I have suffered with these interlinked conditions since I was 6 months old, and I truly know what it is like to experience these debilitating conditions. Every client I have ever worked with has their own triggers and ideal nutrition. There is no such thing as ‘one-size-fits-all’. Whether you work with me one-to-one or use my guided tools, my objective is to help you uncover what works best for you, so that you take back control and experience relief. My guided programmes are only suitable for adults as children have very specific nutrition requirements. I do, however, work with many child clients as part of my clinic. I also offer two free communities for adults caring for children with eczema and digestive symptoms, feel free to come and join us and get some well-deserved support.
To easily keep up with my articles, masterclasses, ebooks and online programmes and receive exclusive access to early bird offers, sign-up to my newsletter. Interested in what I do and who I am? Go to my website: www.jessicafonteneaunutrition.com Sign up for my news to receive the published articles straight to your inbox. Read more by clicking below to see my previously published articles:
I’m Jessica Fonteneau, the Eczema and Digestive Health Nutrition Expert. I’ve worked with hundreds of clients to help them change their diets, better manage their flares, and find relief. My vocation is to help those with eczema and digestive issues, because I have suffered with these interlinked conditions since I was 6 months old, and I truly know what it is like to experience these debilitating conditions. Every client I have ever worked with has their own triggers and ideal nutrition. There is no such thing as ‘one-size-fits-all’. Whether you work with me one-to-one or use my guided tools, my objective is to help you uncover what works best for you, so that you take back control and experience relief. My guided programmes are only suitable for adults as children have very specific nutrition requirements. I do, however, work with many child clients as part of my clinic. I also offer two free communities for adults caring for children with eczema and digestive symptoms, feel free to come and join us and get some well-deserved support.
To easily keep up with my articles, masterclasses, ebooks and online programmes and receive exclusive access to early bird offers, sign-up to my newsletter. Interested in what I do and who I am? Go to my website: www.jessicafonteneaunutrition.com Foods, ingredients, or molecule intolerances appear to be on the rise and whilst some such as gluten or histamine are well known, others, such as salicylates, are more misunderstood. This article will delve into this lesser-known phenomenon exploring:
What are salicylates and what is a salicylate intolerance? Salicylates are natural chemicals found in many plants who use them to defend themselves against pests, bacteria, and environmental stressors. Salicylates are anti-inflammatory and as such have also been synthetically reproduced in laboratories for uses in medications, including aspirin and non-steroidal anti-inflammatories (NSAIDs) such as ibuprofen. Salicylic acid has excellent anti-fungal and anti-bacterial properties, leading to its common use as an ingredient in processed foods, condiments, cosmetics, and beauty products. In terms of food, salicylates are found in many plant foods to a higher or lesser extent. Some of the foods that are common triggers are:
Salicylate intolerance is where a person’s system has difficulty metabolising and tolerating salicylates, leading to a range of symptoms. The phenomenon was initially observed in medically diagnosed patients with either aspirin-exacerbated respiratory disease (AERD) or NSAIDs-exacerbated respiratory disease (NERD) (1,2). In the cases of both AERD and NERD, high doses of chemical salicylates can trigger asthma, rhinosinusitis and urticaria. Clinical case studies have observed that for some, simply eating a diet high in salicylates can contribute to a variety of symptoms, although this can vary from person to person and may also depend on the quantity of salicylates eaten or exposed to over a short period of time. Which symptoms are linked to salicylate intolerance? Whilst respiratory and skin symptoms are the most recognised symptoms of salicylate intolerance, there are others including:
What does the science say causes this condition? As with so many conditions, the exact cause of salicylate intolerance is not well understood, however there are some areas which are being explored:
How is salicylate intolerance medically diagnosed? Diagnosis of salicylate intolerance is tricky, mainly because of the number of overlapping symptoms with other conditions. A medical or nutrition practitioner will undertake:
For many, a salicylate intolerance is linked to other conditions or genetics and is not, itself, the root cause. Sufferers tend to go heavily down the elimination root, which whilst does initially provide relief, is not a sustainable or healthy long-term solution. Working with a practitioner to discover the main trigger of the sensitivity is key. Suggestions for managing a suspected salicylate intolerance.
If on medication, please speak to your GP/consultant before making any changes to your diet. Sign up for my news to receive the published articles straight to your inbox. Read more by clicking below to see my previously published articles:
I’m Jessica Fonteneau, the Eczema and Digestive Health Nutrition Expert. I’ve worked with hundreds of clients to help them change their diets, better manage their flares, and find relief. My vocation is to help those with eczema and digestive issues, because I have suffered with these interlinked conditions since I was 6 months old, and I truly know what it is like to experience these debilitating conditions. Every client I have ever worked with has their own triggers and ideal nutrition. There is no such thing as ‘one-size-fits-all’. Whether you work with me one-to-one or use my guided tools, my objective is to help you uncover what works best for you, so that you take back control and experience relief. My guided programmes are only suitable for adults as children have very specific nutrition requirements. I do, however, work with many child clients as part of my clinic. I also offer two free communities for adults caring for children with eczema and digestive symptoms, feel free to come and join us and get some well-deserved support.
To easily keep up with my articles, masterclasses, ebooks and online programmes and receive exclusive access to early bird offers, sign-up to my newsletter. Interested in what I do and who I am? Go to my website: www.jessicafonteneaunutrition.com References:
|
AuthorI’m Jessica Fonteneau, I’m the eczema specialist and I help people Escape from the Eczema trap. Archives
April 2024
Catégories
All
|





 RSS Feed
RSS Feed